Imagine your liver as a tireless janitor, working 24/7 to detoxify your blood, process nutrients, and regulate energy. Now picture that janitor slowly getting overwhelmed by piles of fat, struggling to function.
Read Also: Late Night Snacking
This is fatty liver disease—a condition where excess fat accumulates in liver cells, often unnoticed until serious damage occurs. Affecting nearly 25% of adults globally, fatty liver is frequently dubbed a “silent epidemic,” with many unaware they have it until routine tests or complications arise. But here’s the good news: It’s often reversible with early action. In this article, we’ll demystify fatty liver, explore its causes, and provide actionable steps to protect—or reclaim—your liver health.
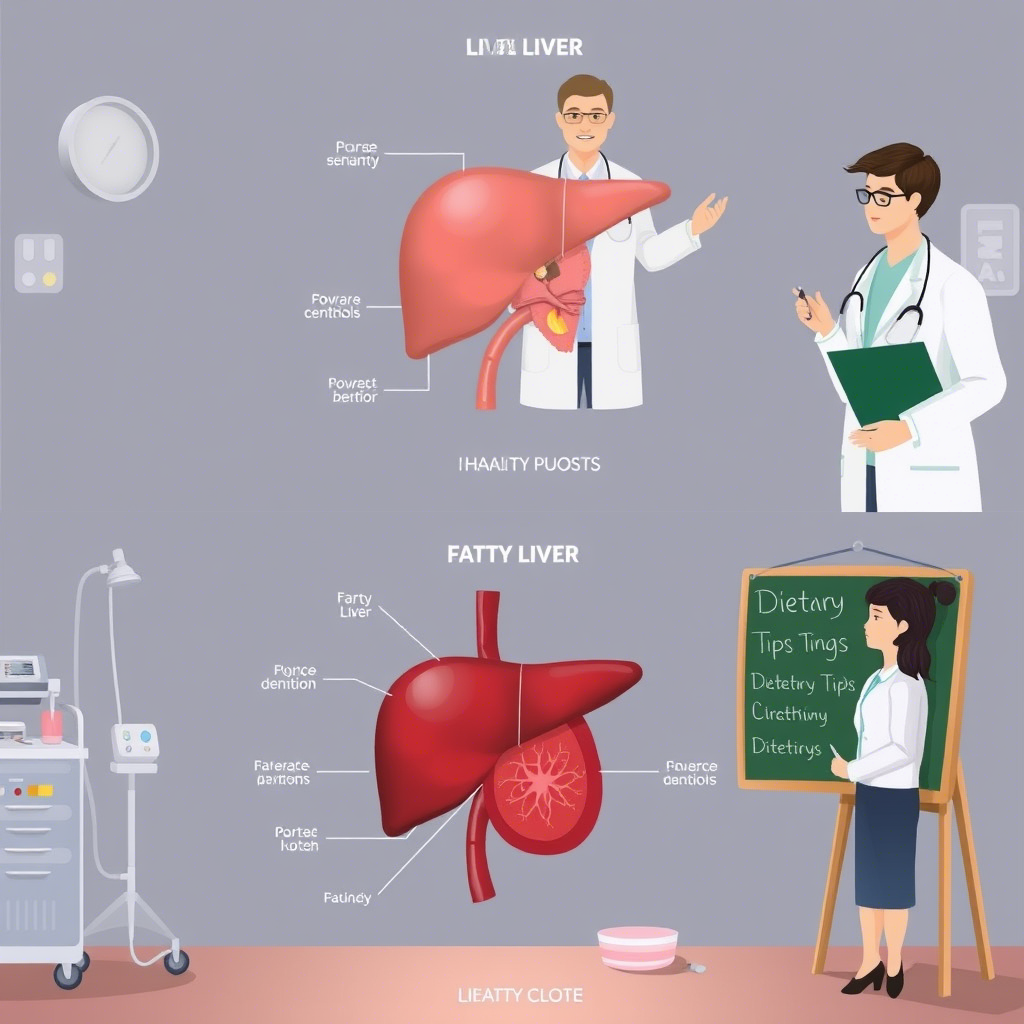
1. Understanding Fatty Liver: More Than Just a Heavy Liver
The Two Faces of Fatty Liver
Fatty liver disease isn’t one-size-fits-all. It has two primary forms:
- Alcoholic Fatty Liver Disease (AFLD): Caused by excessive alcohol consumption, which disrupts liver metabolism.
- Non-Alcoholic Fatty Liver Disease (NAFLD): Linked to metabolic factors like obesity and insulin resistance, even in non-drinkers.
NAFLD is the most common chronic liver disorder worldwide, often coexisting with conditions like type 2 diabetes and high cholesterol.
Subheading: The Silent Progression
Fatty liver typically develops in four stages:
- Simple steatosis: Harmless fat buildup.
- Steatohepatitis (NASH or ASH): Inflammation and liver cell damage.
- Fibrosis: Scar tissue formation.
- Cirrhosis: Severe scarring, leading to liver failure or cancer.
The catch? Stages 1–3 often have no symptoms, making early detection critical.
Subheading: Who’s at Risk?
Risk factors include:
- Obesity (especially abdominal fat).
- Insulin resistance or diabetes.
- High triglycerides or cholesterol.
- Sedentary lifestyle.
- Genetics (family history of liver disease).
2. Causes and Risk Factors: Why Your Liver Holds Onto Fat
Subheading: Alcohol’s Double-Edged Sword
Alcohol is a direct liver toxin. Even short-term binge drinking can cause fat buildup, while chronic use accelerates inflammation and scarring. AFLD is preventable—moderation is key.
Subheading: The Metabolic Syndrome Connection
NAFLD is tightly linked to metabolic syndrome—a cluster of conditions like high blood pressure, high blood sugar, and excess belly fat. Insulin resistance drives the liver to store fat instead of processing it.
Subheading: Hidden Culprits
- Sugar Overload: High fructose intake (e.g., sodas, processed snacks) overwhelms the liver, converting excess sugar to fat.
- Sedentary Habits: Lack of exercise slows metabolism, promoting fat storage.
- Gut Health: An imbalanced gut microbiome may contribute to liver inflammation.
3. Symptoms and Diagnosis: When to Sound the Alarm
Subheading: Early Signs (or Lack Thereof)
Most people with early-stage fatty liver feel perfectly fine. Subtle clues might include:
- Fatigue.
- Mild abdominal discomfort (upper right side).
- Elevated liver enzymes on blood tests (ALT, AST).
Subheading: Diagnostic Tools
- Blood Tests: Check liver enzymes and rule out other causes (e.g., viral hepatitis).
- Imaging: Ultrasound, CT, or MRI detect fat accumulation.
- FibroScan: Measures liver stiffness to assess scarring.
- Biopsy: Gold standard for confirming NASH or fibrosis.
Subheading: Why Early Detection Matters
Catching fatty liver before fibrosis sets in offers the best chance of reversal. Regular check-ups are vital for high-risk individuals.
4. Reversing Fatty Liver: Lifestyle Changes That Work
Subheading: Dietary Interventions
- Ditch Added Sugars: Swap sugary drinks for water, herbal teas, or infused fruits.
- Embrace Whole Foods: Prioritize fiber-rich veggies, lean proteins, and healthy fats (avocados, olive oil).
- Limit Refined Carbs: Choose whole grains over white bread/pasta to stabilize blood sugar.
- Moderate Alcohol: For NAFLD, occasional drinks may be permissible; for AFLD, abstinence is essential.
Subheading: Move Your Body*
Exercise reduces liver fat, even without weight loss:
- Aerobic Exercise: 150 minutes/week of brisk walking, cycling, or swimming.
- Strength Training: Builds muscle, improving insulin sensitivity.
Subheading: Weight Loss—But Not Too Fast*
Losing 5–10% of body weight can significantly reduce liver fat. Crash diets, however, may worsen inflammation. Aim for 1–2 pounds per week.
5. Medical Treatments and Future Hope
Subheading: Current Medications*
No FDA-approved drugs exist specifically for fatty liver, but treatments target underlying conditions:
- Vitamin E: Antioxidant benefits for NASH (under doctor supervision).
- Pioglitazone: Diabetes drug that may reduce liver inflammation.
- Statins: Manage cholesterol, indirectly supporting liver health.
Subheading: Emerging Therapies*
Promising research includes:
- GLP-1 Agonists: Weight-loss drugs showing liver fat reduction.
- FXR Agonists: Medications targeting bile acid pathways.
- Probiotics: Gut-liver axis modulation to reduce inflammation.
Subheading: When to See a Specialist*
Consult a hepatologist if you have:
- Advanced fibrosis or cirrhosis.
- Persistent symptoms despite lifestyle changes.
- Elevated liver enzymes with unknown cause.
FAQs: Your Fatty Liver Questions Answered
Q: Can fatty liver be reversed?
A: Yes! Early-stage fatty liver is often reversible with diet, exercise, and weight loss.
Q: Is NAFLD preventable?
A: Absolutely. Maintaining a healthy weight, exercising, and avoiding excess sugar/alcohol reduce risk.
Q: What foods should I avoid?
A: Limit fried foods, sugary snacks, refined carbs, and processed meats.
Q: Can skinny people get fatty liver?
A: Yes. “Lean NAFLD” affects up to 20% of cases, often linked to insulin resistance.
Q: How often should I get tested?
A: Annual check-ups if you have risk factors; discuss with your doctor.
Conclusion
Fatty liver isn’t a life sentence—it’s a wake-up call. By understanding its stealthy nature and addressing root causes like diet, inactivity, and metabolic health, you can reclaim control of your liver. Progress, not perfection, is the goal. Small, consistent changes—swapping soda for sparkling water, taking daily walks, prioritizing sleep—add up to transformative results.
Final Thought:
Your liver is a resilient organ, capable of regeneration even after significant damage. Treat it with care, and it’ll return the favor by keeping you healthy for decades to come.

Pingback: Insulin Resistance - Mental Health Stigma